Bugs, Bites, and Stings
Esteban Faith-Fernandez
Kenneth J. Tomecki
Published: April 2012
Scabies
Definition and Etiology
Scabies is an ectoparasite infestation caused by the female mite Sarcoptes scabiei var. hominis. Norwegian scabies is a more severe infestation found in immunocompromised patients with decreased sensory function and in institutionalized persons.
Prevalence and Risk Factors
The prevalence varies with location, but children and teenagers are most commonly affected. Risk factors include low socioeconomic status, crowded living conditions, and limited access to water.
Pathophysiology and Natural History
Transmission usually occurs by close body contact. Clothing and bedding occasionally act as fomites for transmission. The female mite burrows into the epidermis at a rate of 0.5 to 5 mm/day, lives for 4 to 6 weeks, and produces 2 to 4 eggs daily. An infested patient usually harbors less than 15 mites.
Signs, Symptoms, and Diagnosis
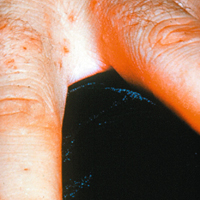
In primary cases, signs and symptoms occur several weeks after infestation. In subsequent episodes, hypersensitivity reactions can develop within a day. Pruritus is usually severe and most prominent at night. Typical skin disease is erythematous papules and vesicles in the interdigital spaces, flexural surface of the wrists and elbows, axillae, areolae, and genitals (Figs. 1 and 2). Face, scalp, and neck are rarely affected except in infants and children. Secondary changes, such as excoriations, eczema, and secondary infection, often follow, especially if disease is persistent.
The burrow—a 1- to 10-mm threadlike plaque—is pathognomonic for scabies, though it is not always easily identified. Reddened nodules can develop on the elbows, anterior axillary folds, penis, and scrotum; these represent a hypersensitivity reaction that can persist for weeks. Itching and the presence of flexural vesicles and burrows should suggest the diagnosis. Identification of the scabies mite, eggs, or fecal pellets from skin scrapings confirms the diagnosis.
Treatment
Permethrin 5% cream (Elimite) is the treatment of choice for uncomplicated scabies in adults, including pregnant women, and in children as young as 1 month. The cream is applied to the trunk and extremities, washed off after 8 to 14 hours, then followed by a second application 7 days later. This routine is approximately 95% successful.
Although it is not yet approved as a treatment for scabies, ivermectin has proved to be very effective. The usual dose is 200 μg/kg as a single dose, then repeated in 10 to 14 days. Its safety has not been proved in pregnancy or in children who weigh less than 15 kg.
Prevention
Close contacts deserve treatment even in the absence of symptoms. Bed linen and clothing should be washed in hot water and dried on high heat, or it may simply be placed in closed plastic bags for 5 to 7 days.
Considerations in Special Populations
Crusted scabies, also known as Norwegian scabies, is a hyperinfestation with thousands of mites that results from the host’s inability to mount an immune response to control the infestation. Those at risk are patients with HIV infection, leprosy, hematologic malignancy, graft-versus-host disease, or immunosuppressive therapy; patients with nutritional disorders; and patients with Parkinson’s disease, Down’s syndrome, and mental retardation.
Crusted scabies, with its hyperkeratotic plaques or nodules, has a predilection for the hands and feet, often resembling psoriasis. Despite the dramatic skin disease and the number of mites, pruritus is usually mild, but lymphadenopathy and eosinophilia can occur.
Crusted scabies is highly infectious, and prompt diagnosis and treatment are essential. Affected patients deserve treatment with permethrin and ivermectin, coupled with vigorous cleaning of clothing and bedding.
Summary
- Scabies is caused by the female mite Sarcoptes scabiei var. hominis.
- Diagnosis is based on clinical presentation and demonstration of the mite or eggs (or both) microscopically.
- Permethrin 5% cream is the treatment of choice for uncomplicated scabies, coupled with treatment of close contacts, bed linen, and clothing.
- Crusted scabies is a hyperinfestation in compromised persons unable to mount an appropriate immune response.
Pediculosis
Lice produce three main infestations in humans, depending on the affected body site: pediculosis capitis (head), corporis (body), and pubis (perineum).
Definition and Etiology
Head lice (pediculosis capitis) is caused by the louse Pediculus humanus var. capitis; Pediculus humanus var. humanus is responsible for body lice. The crab louse, Phtirus pubis, infests the pubic hair and occasionally the eyelashes, beard, and axillae.
Prevalence and Risk Factors
Head lice infestation occurs worldwide, with a reported incidence of 12 million cases per year in the United States. It primarily affects children aged 3 to 11 years. It affects all socioeconomic and ethnic groups, less so African Americans.
Body lice occurs in people living in crowded, often unsanitary conditions, such as homeless persons and refugees.
Pubic lice primarily affects sexually active persons, particularly teenagers and young adults.
Pathophysiology and Natural History
Transmission of all forms of human lice requires close contact. Head lice are transmitted by head-to-head contact; it is transmitted less often by fomites. Pubic lice is transmitted by sexual, contact with an infested partner, or less so by contact with the infested person’s bed linens, towels, or clothes. Body lice are transmitted by contact with infested persons, who usually live in close, crowded conditions and cannot bathe or change clothes regularly. Head lice and pubic lice or their eggs or nits attach to hairs. body lice live and lay eggs in clothing, not on humans.
Signs, Symptoms, and Diagnosis
Pruritus is the hallmark of all forms of lice. Eczematous changes and secondary infection can follow a patient’s scratching. The presence of lice or nits (nodularities on the hair) establishes the diagnosis (Fig. 3). The presence of nits alone can simply indicate past infestation. Brushing with a fine-toothed comb can enhance detection of head lice. Pubic lice often produce bluish macules (maculae ceruleae) on the buttocks, upper thighs, and lower abdomen; these macules are thought to be hemosiderin deposition at the site of bites.
Treatment
For head lice, current recommendations include permethrin 1% cream, lindane 1%, or pyrethrins, each applied to a dry scalp for 5 to 10 minutes, followed by rinsing. Malathion 0.5% applied for 8 to 12 hours, then rinsed off can also be used. Each approach should be repeated in 1 week.
For body lice, laundering of clothes and linens coupled with enhanced hygiene is also essential.
For pediculosis pubis, treatment options include permethrin 1% cream applied for 10 minutes or lindane 1% applied for 4-5 minutes or a pyrethrin with piperonyl butoxide applied for 10 minutes, followed by rinsing.
In addition, bedding and clothing should be machine washed and dried with high heat. Close contacts and sexual partners should be treated in similar fashion. Affected patients should be evaluated for other sexually transmitted diseases.
Lindane is not recommended as treatment of infestations in children younger than 2 years and in pregnant women.
Summary
- Head lice (pediculosis capitis) is caused by Pediculus humanus var. capitis.
- Body lice (pediculosis corporis) is caused by Pediculus humanus var. humanus.
- Pubic lice (pediculosis pubis) is caused by Pthirus pubis.
- Pruritus is the hallmark of all lice infesations.
- Pubic lice should raise the possibility of other coexistent sexually transmitted diseases.
Bedbugs
Definition and Etiology
Bedbugs are blood-sucking insects of the order Cimicidae. The most common species is Cimex lenticularis.
Pathophysiology and Natural History
Bedbugs typically feed on sleeping persons, attracted by their body temperature and carbon dioxide production. They tend to live under carpets or floorboards and along the seams of mattresses. They feed infrequently but can live for 1 year. Bedbug resurgence has occurred within the last decade.
Signs, Symptoms, and Diagnosis
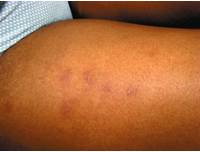
Bedbug bites vary from itchy erythematous macules to itchy indurated papules, wheals, vesicles, or bullae, usually on exposed areas of the face, neck, and extremities. They tend to resolve within 2 weeks (Fig. 4). Bites often occur in groups of three, known as the “breakfast, lunch, dinner” pattern. Bedbugs do not transmit diseases.
Treatment
Treatment of patients with bedbug bites is symptomatic, usually nothing more than topical coritocosteroids. Pesticides with dichlorvos, malathion, and pyrethrins are effective in eliminating bedbugs. Prevention of infestation can be achieved with repellents or permethrin-impregnated bed nets.
Summary
- Cimex lenticularis is the most common bedbug.
- An itchy nighttime dermatitis, especially grouped papules, should suggest bedbug bites.
- Treatment is symptomatic, such as topical corticosteroids.
Fire Ants
Definition and Etiology
Fire ants include the red fire ant (Solenopsis invicta) and the black fire ant (Solenopsis richteri). They are well established in the southeastern United States after their importation from South America in the early 20th century. Approximately 30% to 60% of residents in that area are stung every year.
Signs, Symptoms and Diagnosis
Fire ants are aggressive critters, attacking in groups when the anthill is disturbed. The initial bite or sting has a burning sensation followed by an erythematous wheal-and-flare reaction. Within hours, sterile pustules form at the sites of the stings. The pustules are commonly arranged in a rosette or ring pattern, because the ants bite, then pivot and sting in a circular fashion. True anaphylaxis affects 1% of affected persons, usually within hours of the sting.
Treatment
Local reactions deserve symptomatic treatment with compresses, elevation of the affected extremity, and topical corticosteroids. For anaphylactic reactions, immunotherapy with imported fire ant whole body extract has been effective in selected cases.
Summary
- Fire ants (Solenopsis invicta and Solenopsis richteri) are endemic in the southeastern United States.
- Sterile pustules are the characteristic clinical finding, usually with a burning or stinging sensation.
- Anaphylactic reactions occur in 1% of stung persons.
Cutaneous Myiasis
Definition and Etiology
Cutaneous myiasis, an infestation by larvae of the order Diptera, has three main clinical patterns: furuncular myiasis, wound myiasis, and migratory myiasis. Dermatobia hominis (the human bot fly) is the most common agent of cutaneous and furuncular myiasis in North America, usually occurring in travelers from Central and South America, where the fly is common. Though rare, the most common cause of US-acquired furuncular myiasis is the rodent or rabbit bot fly of the genus Cuterebra. Wound myiasis is most commonly caused by Cochliomyia hominivorax.
Prevalence and Risk Factors
Wound myiasis is the most common type of myiasis in the United States. Risk factors include advanced age, poor social and hygiene conditions, open wounds, psychiatric illness, alcoholism, diabetes, and vascular occlusive disease. Travel to tropical and subtropical areas is the main risk factor for furuncular and migratory myiasis.
Pathophysiology and Natural History
The mode of transmission varies among genera. The adult female bot fly lays eggs on foliage or insects (mosquitoes, flies, ticks), which are then transferred to human skin by direct contact with foliage or biting insects. Once the larva hatches, it burrows into the skin.
Signs, Symptoms, and Diagnosis
Furuncular myiasis exhibits solitary or multiple boil-like nodules on exposed skin, occasionally with drainage (serosanguineous or seropurulent) and surrounding erythema. Patients often have pruritus and local tenderness, and sometimes the larva can be seen protruding from a central pore (Fig. 5). When the nodule is submerged, bubbling occurs if the larva is still alive.
Patients with creeping or migratory myiasis have pruritic, linear, reddened, serpentine plaques, which differ from cutaneous larva migrans in that it extends more slowly. The fly larvae are usually larger in size and survive longer.
In wound myiasis, larvae are readily visualized with varying degrees of tissue destruction. Larvae can invade mucous membranes and body cavities.
Diagnosis of cutaneous myiasis is based on the clinical presentation and presence of the larvae.
Treatment
Removal of the larvae is curative in all cases. The nodule can be occluded by application of a substance (e.g., petrolatum, nail polish, animal fat, beeswax, paraffin, mineral oil) to asphyxiate the larva and force its exit. The larva can be removed manually or mechanically. Larvicides (topical or oral e.g., ivermectin), mineral turpentine, ethanol spray, and oil of betel leaf kill the larva, which can then be removed.
Summary
- Cutaneous myiasis is an infestation by larvae of the order Diptera.
- There are three types of myiasis: furuncular, wound and migratory or creeping.
- Treatment requires removal of the larva by occlusion, by manual or mechanical means, or with larvicides.
Cutaneous Larva Migrans
Definition and Etiology
Cutaneous larva migrans (CLM) is an infestation by a nematode, most often the animal hookworm (Ancylostoma caninum or Ancylostoma braziliense), less often the human hookworm (Ancylostoma duodenale and Necator americanus).
CLM occurs most commonly in areas with warm climates such as Africa, Asia, Latin America, and the southeastern United States. It is the most common travel-related skin disease, often occurring in travelers who have visited these areas.
Pathophysiology and Natural History
CLM is a self-limited disease, invariably acquired when the skin has contact with sand or soil contaminated with animal feces. The feet are the most common affected site, and the legs and buttocks are less so. Left untreated, the disease resolves within a few months.
Signs, Symptoms, and Diagnosis
Affected patients have itchy erythematous, serpiginous tracks, usually on the feet, buttocks, or thighs (Fig. 6). The track advances 1 to 2 cm/day.
The history and pattern of skin disease (serpiginous tracks) and its location should suggest the diagnosis.
CLM must be clinically differentiated from migratory myiasis and cutaneous larva currens. Migratory myiasis extends more slowly; the fly larvae are usually larger and survive longer. Cutaneous larva currens is the infestation with the roundworm Strongyloides stercoralis. The sign is pruritic, serpiginous, erythematous tracks on the perineal area, buttocks, and thighs, which evolve rapidly at a rate of 5 to 15 cm/hr. This differentiation is important, because cutaneous larva currens may be associated with systemic or disseminated infection with a mortality rate of up to 70% to 90%
Treatment
Several treatment strategies exist. The most common treatments are thiabendazole cream 2 or 3 times a day for 5 to 10 days, albendazole 400 mg orally daily for 3 to 5 days, and ivermectin as a single dose of 12 mg (200 μg/kg).
Summary
- CLM is the most common travel-related skin disease.
- CLM is caused by a nematode (hookworm).
- Itchy, reddened, serpiginous tracks on the feet or buttocks are characteristic findings.
- Anthelminthics, either topical or oral, are the treatment of choice.
Seabather’s Eruption
Definition and Etiology
Seabather’s eruption, or sea lice, is an acute dermatitis that begins after exposure to seawater containing the thimble jellyfish Linuche unguiculata. The eruption is a dermatitis caused by the sting of the jellyfish larvae trapped within a bathing suit.
Prevalence and Risk Factors
Seabather’s eruption occurs in the spring and summer, most commonly along the coasts of Florida and in the Caribbean. Children, surfers, and those with a prior occurrence are most commonly affected.
Signs, Symptoms and Diagnosis
Within 24 hours after exposure to infested seawater, erythematous macules, papules, or wheals appear on areas of the body that were covered by the bathing suit) (Fig. 7). The dermatitis results from the firing of the nematocyst after a change in osmotic pressure. Occasionally, systemic symptoms (fever, chills, nausea, headache) occur, particularly in children and adolescents. The dermatitis resolves in 7 to 10 days. The diagnosis is based on the clinical appearance of the dermatitis on covered skin after seawater exposure.
Treatment
Treatment is symptomatic and consists of antihistamines and topical corticosteroids. Severe cases can require systemic corticosteroids. Removal of the bathing suit and showering after seawater exposure is protective.
Summary
- Seabather’s eruption is a dermatitis caused by stings of the larval form of the jellyfish Linuche unguiculata.
- The dermatitis appears on covered areas after seawater exposure.
Swimmer’s Itch
Definition, Etiology and Risk Factors
Swimmer’s itch, or cercarial dermatitis, is a pruritic skin disease caused by penetration of cercariae (trematode larvae of the genera Schistosoma and Trichobilharzia). These larvae are common in fresh water (lakes, ponds) and occasionally in salt water.
Cercarial dermatitis is common in children during the summer months after exposure to fresh water, particularly in shallow waters.
Signs, Symptoms and Diagnosis
A few hours after cercarial contact, a pruritic monomorphic dermatitis appears, characterized by erythematous macules and papules on uncovered skin. The larvae die within few hours, and the dermatitis spontaneously resolves in 1 to 2 weeks, even without treatment.
Treatment
Treatment is symptomatic with antihistamines and topical corticosteroids. For severe, generalized disease, systemic glucocorticoids may be necessary.
Summary
- Swimmer’s itch (cercarial dermatitis) is caused by invasion of the skin by larvae of trematodes, usually acquired in fresh water.
- Skin disease is essentially a dermatitis on exposed skin after fresh water contact, e.g. swimming.
Suggested Readings
- deShazo RD, Butcher BT, Banks WA: Reactions to the stings of the imported fire ant. N Engl J Med 1990;323(7):462-466.
- Galiczynski EM Jr, Elston DM: What’s eating you? Pubic lice (Pthirus pubis). Cutis 2008;81(2):109-114.
- Heukelbach J, Feldmeier H: Epidemiological and clinical characteristics of hookworm-related cutaneous larva migrans. Lancet Infect Dis 2008;8(5):302-309.
- Heukelbach J, Feldmeier H: Scabies. Lancet 2006;367(9524):1767-1774.
- Jacobson CC, Abel EA: Parasitic infestations. J Am Acad Dermatol 2007;56(6):1026-1043.
- Kumar S, Hlady WG, Malecki JM: Risk factors for seabather’s eruption: A prospective cohort study. Public Health Rep 1997;112(1):59-62.
- Lebwohl M, Clark L, Levitt J: Therapy for head lice based on life cycle, resistance, and safety considerations. Pediatrics 2007;119(5):965-974.
- McGraw TA, Turiansky GW: Cutaneous myiasis. J Am Acad Dermatol 2008;58(6):907-926.
- Mumcuoglu KY, Barker SC, Burgess IE, et al: International guidelines for effective control of head louse infestations. J Drugs Dermatol 2007;6(4):409-414.
- Steen CJ, Carbonaro PA, Schwartz RA: Arthropods in dermatology. J Am Acad Dermatol 2004;50(6):819-842.
- Strong M, Johnstone PW: Interventions for treating scabies. Cochrane Database Syst Rev 2007;(3):CD000320.
- Ter Poorten MC, Prose NS: The return of the common bedbug. Pediatr Dermatol 2005;22(3):183-187.
- Verbrugge LM, Rainey JJ, Reimink RL, Blankespoor HD: Prospective study of swimmer’s itch incidence and severity. J Parasitol 2004;90(4):697-704.