Liver Test Interpretation – Approach to the Patient with Liver Disease: A Guide to Commonly Used Liver Tests
Arvind R. Murali
William D. Carey
Published: April 2014
Laboratory assessment of the patient with suspected or clinically obvious liver disease is context dependent. For example, the acutely ill jaundiced patient with a history of prolonged alcohol ingestion requires a different laboratory assessment than the well patient in whom one or more standard liver test results are discovered to be abnormal during routine testing. Additionally, the sequence of liver tests depends heavily on the questions being asked. If it is to determine whether this well person whose brother was recently diagnosed with hemochromatosis also has this genetic disease, then a series of tests will be initiated to detect the possibility of iron overload. If it is to determine whether this spouse has been infected with hepatitis B, then blood tests related to hepatitis B will be required. Thus generic algorithms for the evaluation of liver disease need to be considered skeptically.
This chapter is intended to discuss a useful way of thinking about liver tests. It emphasizes limitations of and alternative explanations for isolated abnormalities of common liver test results. It also provides information on the initial screening test to be chosen, their interpretation, and the tests needed to confirm the diagnosis of common liver disorders based on current recommendations. Information in this chapter should be combined with discussions of specific liver diseases in the Disease Management. A final caveat relates to terminology. Tests done in clinical laboratories do not measure any functional capacity of the liver. Hence, the commonly used term liver function test is inaccurate, and the term liver tests is used in this chapter. Guidelines on the interpretation and evaluation of abnormal liver test results have been published.1,2 Useful algorithms are presented that parallel the recommendations in this chapter.
Isolated Abnormalities in Liver Test Results
A common clinical scenario is the unanticipated discovery of an abnormal liver test result, obtained when a bundle of tests has been done for other reasons. Most clinical laboratories offer bundled blood tests, which often contain all or most of the following:
- Bilirubin
- Aspartate transaminase (AST, formerly referred to as serum glutamic-oxaloacetic transaminase, SGOT)
- Alanine transaminase (ALT, formerly called serum glutamic-pyruvic transaminase, SGPT)
- Gamma-glutamyl-transpeptidase (GGTP)
- Alkaline phosphatase
- Lactate dehydrogenase (LDH)
Of these tests only the GGTP is liver specific. An isolated elevation of just one of the other test values should raise suspicion that a source other than the liver is the cause (Table 1). When several liver test results are simultaneously out of the normal range, consideration of non-hepatic sources becomes irrelevant.
Table 1: Nonhepatic Sources of Abnormalities for Select Laboratory Tests
| Test | Nonhepatic Source |
|---|---|
| Bilirubin | Red blood cells (e.g., hemolysis, intra-abdominal bleed, hematoma) |
| AST | Skeletal muscle, cardiac muscle, red blood cells |
| ALT | Skeletal muscle, cardiac muscle, kidneys |
| LDH | Heart, red blood cells (e.g., hemolysis) |
| Alkaline phosphatase | Bone, first trimester placenta, kidneys, intestines |
ALT, alanine aminotransaminase; AST, aspartate transaminase; LDH, lactate dehydrogenase.
Additional note should be made of the GGTP and LDH as liver tests. The GGTP level is too sensitive, frequently elevated when no liver disease is apparent. A GGTP test is useful in only two instances: (1) It confers liver specificity to an elevated alkaline phosphatase level; (2) In aminotransferase level elevations with AST/ALT ratio greater than 2, elevation of GGTP further supports alcoholic liver disease. In addition, it can be used to monitor abstinence from alcohol. An isolated elevation of the GGTP level does not need to be further evaluated unless there are additional clinical risk factors for liver disease.3 The LDH assay is insensitive and nonspecific because LDH is present in tissues throughout the body.
Evaluation of Liver Disease Based on Enzyme Levels
It is customary and useful to categorize liver diseases into three broad categories: Hepatocellular, in which primary injury is to the hepatocytes; cholestatic, in which primary injury is to the bile ducts; and infiltrative, in which the liver is invaded or replaced by non-hepatic substances, such as neoplasm or amyloid. Although there is a great deal of overlap in liver test result abnormalities seen in these three categories, particularly in cholestatic and infiltrative disorders, an attempt to characterize an otherwise undifferentiated clinical case as hepatocellular, cholestatic, or infiltrative often makes subsequent evaluation faster and more efficient. The AST, ALT, and alkaline phosphatase tests are most useful to make the distinction between hepatocellular and cholestatic disease.
The normal range for aminotransferase levels in most clinical laboratories is much lower than that for the alkaline phosphatase level. Accordingly, when considering levels of elevations, it is necessary to consider them relative to the respective upper limit of normal for each test compared. Consider a patient with an AST level of 120 IU/mL (normal, ≤40 IU/mL) and an alkaline phosphatase of 130 IU/mL (normal, ≤120 IU/mL). This represents a hepatocellular pattern of liver injury because the AST level is three times the upper limit of normal, whereas the alkaline phosphatase level is only marginally higher than its upper limit of normal.
Serum aminotransferase levels—ALT and AST—are two of the most useful measures of liver cell injury, although the AST is less liver specific than is ALT level. Elevations of the AST level may also be seen in acute injury to cardiac or skeletal muscle. Lesser degrees of ALT level elevation may occasionally be seen in skeletal muscle injury or even after vigorous exercise. Thus in clinical practice, it is not uncommon to see elevations of AST, ALT or both in common non-hepatic conditions such as myocardial infarction and rhabdomyolysis. Diseases that primarily affect hepatocytes, such as viral hepatitis, will cause disproportionate elevations of the AST and ALT levels compared with the alkaline phosphatase level. The ratio of AST/ALT is of little benefit in sorting out the cause of liver injury except in acute alcoholic hepatitis, in which the ratio is usually greater than 2.
The current upper limit of serum ALT, though varied among laboratories, is generally around 40 IU/L. However, recent studies have shown that the upper limit threshold of ALT level should be lowered because people who have slightly raised ALT levels that are within the upper limit of normal (35-40 IU/L) are at an increased risk of mortality from liver disease.4 In addition, it has been suggested that gender-specific thresholds be applied because women have slightly lower normal ALT levels than men. One such study conducted in the U.S. identified an ALT upper limit of 29 IU/L for men and 22 IU/L for women.5 In asymptomatic patients with minimal elevations of aminotransferases, it is reasonable to repeat the test in a few weeks to confirm elevation. Common causes of mild increases in AST and ALT levels include non-alcoholic fatty liver disease (NAFLD), hepatitis C, alcoholic fatty liver disease, and medication effect (e.g., due to statins).
Serum alkaline phosphatase comprises a heterogeneous group of enzymes. Hepatic alkaline phosphatase is most densely represented near the canalicular membrane of the hepatocyte. Accordingly, diseases that predominately affect hepatocyte secretion (e.g., obstructive diseases) will be accompanied by elevations of alkaline phosphatase levels. Bile-duct obstruction, primary sclerosing cholangitis, and primary biliary cirrhosis (PBC) are some examples of diseases in which elevated alkaline phosphatase levels are often predominant over transaminase level elevations (Table 2).
Table 2: Category of Liver Disease by Predominant Serum Enzyme Abnormality
| Liver Disease Category
|
|||
|---|---|---|---|
| Test | Hepatocellular | Cholestatic | Infiltrative |
| AST, ALT higher than alkaline phosphatase level | Typical | — | — |
| Alkaline phosphatase higher than AST, ALT levels | — | Typical | — |
| Elevation of alkaline phosphatase with near-normal AST, ALT levels | — | Typical | Typical |
ALT, alanine aminotransaminase; AST, aspartate transaminase.
Infiltrative liver diseases most often result in a pattern of liver test result abnormalities similar to those of cholestatic liver disease. Differentiation often requires liver imaging studies. Liver imaging by ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) most often identify infiltration of the liver by mass lesions such as tumors. Imaging by cholangiography—endoscopic retrograde cholangiography, transhepatic cholangiography, or magnetic resonance cholangiography—identifies many bile duct lesions that cause cholestatic liver disease. Liver biopsy is often needed to confirm certain infiltrative disorders (e.g., amyloidosis) and microscopic biliary disorders such as PBC.
Bilirubin Level Elevations
Bilirubin is produced by the normal breakdown of pigment-containing proteins, especially hemoglobin from senescent red blood cells and myoglobin from muscle breakdown. Bilirubin released from such sources, tightly albumin bound, is delivered to the liver, where it is efficiently extracted and conjugated by hepatic glucuronidation and sulfation. Conjugated bilirubin is rapidly excreted into bile and removed from the body through the gut. Therefore, the amount of conjugated bilirubin present in serum in healthy subjects is trivial (<10% of measured total bilirubin). An elevated level of conjugated serum bilirubin implies liver disease. Also, it is important to note that only conjugated bilirubin appears in urine (unconjugated bilirubin is albumin bound and water insoluble). The presence of bilirubin in urine almost always implies liver disease.
Many laboratories report only the total bilirubin level, the sum of the conjugated and unconjugated portions. It is sometimes useful to determine the fraction of total serum bilirubin that is unconjugated versus that which is conjugated, usually referred to as fractionation of bilirubin. This is most useful when all the standard liver test results are normal, except the total bilirubin. To make matters more confusing, the conjugated bilirubin is sometimes referred to as the direct-reacting bilirubin and the unconjugated as the indirect-reacting bilirubin (Table 3).
Table 3: Bilirubin Fractions Present in Blood and Urine
| Fraction | In Serum As | Measured As | Present in Urine |
|---|---|---|---|
| Unconjugated | Albumin-bound | Indirect-reacting bilirubin | Never |
| Conjugated | Unbound | Direct-reacting bilirubin | Yes, when serum bilirubin level is elevated |
Normally, 90% or more of measured serum bilirubin is unconjugated (indirect-reacting). When the total bilirubin level is elevated and fractionation shows that the major portion (≥90%) is unconjugated, liver disease is never the explanation. Instead, the clinician should suspect one of two explanations: Gilbert disease or hemolysis. If the patient is young and healthy, an inherited decrease in the inability to conjugate bilirubin is likely and is referred to as Gilbert syndrome. It is seen in about 5% of the general population and causes only mild hyperbilirubinemia without symptoms. It is not associated with liver disease. Interestingly, fasting and intercurrent illnesses such as influenza often make the level of unconjugated bilirubin even higher in those with Gilbert syndrome. This syndrome is easily diagnosed when all standard liver-test results are normal and 90% or more of the total bilirubin is unconjugated. There is no need for an imaging study or liver biopsy in cases of suspected Gilbert syndrome.
Elevations of the unconjugated bilirubin level when the conjugated bilirubin level remains normal may also indicate an increased load of bilirubin caused by hemolysis. Anemia and an elevated reticulocyte count are usually present in such cases (Table 4).
Table 4: Common Causes of Isolated Bilirubin Elevation
| Cause | Direct-Reacting Bilirubin | Indirect-Reacting Bilirubin | Associated Features |
|---|---|---|---|
| Liver disease (many types) | Elevated | Elevated or normal | Liver enzyme levels often elevated |
| Hemolysis | Normal | Elevation represents more than 90% of total bilirubin | Anemia usual; increased reticulocyte count; normal liver enzyme levels (although LDH may be elevated) |
| Gilbert’s syndrome | Normal | Elevation represents more than 90% of total bilirubin (common) | No abnormal liver tests; no anemia; onset in late adolescence; fasting makes bilirubin rise |
LDH, lactate dehydrogenase.
Many clinicians mistakenly interpret elevations of direct-reacting bilirubin to indicate that cholestatic (obstructive) liver disease is present. It is apparent from Table 2 that the serum bilirubin level plays no useful role in categorizing a case as hepatocellular, cholestatic, or infiltrative. The bilirubin level may be normal or elevated in each type of disorder. Viral hepatitis A, a prototypic hepatocellular disease, may frequently be associated with bilirubin levels that are high, whereas PBC, a prototypic cholestatic disorder, is associated with a normal serum bilirubin level except in later stage disease. Serum bilirubin levels should be disregarded when trying to decide whether the liver-test pattern is more suggestive of hepatocellular or cholestatic disease.
Determination of Specific Liver Disorders
Acute Alcoholic Hepatitis
Acute alcoholic hepatitis may be mild or life threatening. The pattern of liver test abnormality is hepatocellular. The AST is typically in the 100 to 200 IU/L range, even in severe disease, and the ALT level may be normal, even in severe cases. The AST level is higher than the ALT level, and the ratio is greater than 2:1 in 70% of patients. A ratio greater than 3 is strongly indicative of alcoholic hepatitis. An important corollary is that an AST greater than 500 IU/L or an ALT greater than 200 IU/L is not likely to be explained by acute alcoholic hepatitis—even in an alcoholic patient—and should suggest another etiology.6
The degrees of bilirubin level increase and prothrombin time elevation are better indicators of severity of disease. In alcoholic hepatitis, the Maddrey discriminant function (MDF), a disease-specific prognostic score which indicates the severity of liver injury, has been developed. The formula to calculate the score is as follows:
MDF = 4.6 (patient’s prothrombin time − control prothrombin time) + total bilirubin (mg/dL)
Patients who have a score of 32 or greater have an increased risk of death, with a 1-month mortality rate of 30% to 50%.
Viral Hepatitis
Viral hepatitis most often produces a hepatocellular pattern of injury (AST and ALT level elevations predominate). Patients who have no symptoms and in whom aminotransferase levels are normal may still be infected. In addition, a great deal of confusion is caused by abnormal viral markers, many of which do not indicate active infection but rather immunity. These concepts are more fully developed elsewhere in the Cleveland Clinic Disease Management.
Hepatitis A
Hepatitis A virus (HAV) infection is an acute, self-limited disease in most cases, although it may rarely be fatal. Diagnosis is made through the use of antibody tests (anti-HAV). Positive anti-HAV IgM antibody is diagnostic of acute hepatitis A infection and has a very good sensitivity and specificity. The IgM antibodies are usually positive at the time of the onset of symptoms and they remain positive for about 3 to 6 months after, and in some cases as long as 1 year. Anti-HAV immunoglobulin G (IgG) antibodies develop later than anti-HAV immunoglobulin M (IgM) but they persist for many years and offer immunity. Anti-HAV IgG antibodies are also seen following vaccination.
The presence of anti-HAV IgM—irrespective of the presence of anti-HAV IgG—suggests acute infection. The presence of anti-HAV IgG in the absence of IgM suggests previous infection or post-vaccination antibodies.
When an acute hepatitis A panel is ordered, the test result that is obtained from the laboratory must be interpreted with caution before making the diagnosis. This is because the standard screening tests performed by most laboratories measure the level of total anti-HAV antibodies. Total anti-HAV antibody tests will be positive in the presence of either anti-HAV IgG or IgM, as the reagents used in this test will react to both anti-HAV IgG and IgM. Therefore, a positive total anti-HAV antibody test alone does not provide the diagnosis of acute hepatitis A. Selective testing of serum IgM anti-HAV is required to establish such a diagnosis (Table 5).
Table 5: Hepatitis A Antibody Testing In Different Clinical States
| State | Total Anti-HAV (IgG, IgM) | Anti-HAV IgM |
|---|---|---|
| Acute hepatitis A | Positive | Positive |
| Resolved hepatitis A | Positive | Negative |
| Immunization | Positive | Negative |
HAV, hepatitis A virus; IgG, immunoglobulin G; IgM, immunoglobulin M.
Hepatitis B
Like hepatitis A, hepatitis B in adults produces hepatocellular enzyme level elevations (AST and ALT predominate). In adults who acquire hepatitis B, the infection almost always clears, but antibodies persist. In a few, the disease does not resolve but becomes chronic. These patients retain serum markers of viral infection. Many blood tests are available for hepatitis B antigenic determinants and their antibodies. It is best to separate testing appropriate for the acute hepatitis situation from testing for chronic liver disease caused by hepatitis B. Only a few tests need to be considered by the generalist to determine the status of a patient with possible hepatitis B. A full discussion of hepatitis B can be seen in the Disease Management chapter on Hepatitis B.
Acute Hepatitis B
Hepatitis B surface antigen (HBsAg) emerges within 2 weeks of exposure but can often be delayed for weeks or months. This antigen is present in the blood for a variable period, usually encompassing the time during which the patient is clinically ill and most likely to seek medical attention. In patients with mild symptoms whose testing may be delayed, the HBsAg level may have already declined. In this case, a second chance to make the diagnosis comes from detection of the IgM antibody directed against the hepatitis B core (HBc) antigen, anti HBc-IgM (Table 6). Similar to the testing for acute hepatitis A, selective testing of serum IgM anti-HBc is required to establish a diagnosis of acute hepatitis B in patients whose HBsAg levels have already declined. The total anti-HBc antibody test will be positive in the presence of either anti-HBc IgG or IgM.
Table 6. Common Hepatitis B Testing Results
| Test | Result | Interpretation |
|---|---|---|
| HBsAg | Negative | Susceptible |
| Anti-HBc | Negative | |
| Anti-HBs | Negative | |
| HBsAg | Negative | Immune due to natural infection |
| Anti-HBc | Positive | |
| Anti-HBs | Positive | |
| HBsAg | Negative | Immune due to hepatitis B vaccination |
| Anti-HBc | Negative | |
| Anti-HBs | Positive | |
| HBsAg | Positive | Acutely infected |
| Anti-HBc | Positive | |
| IgM anti-HBc | Positive | |
| Anti-HBs | Negative | |
| HBsAg | Positive | Chronically infected |
| Anti-HBc | Positive | |
| IgM anti-HBc | Negative | |
| Anti-HBs | Negative | |
| HBsAg | Negative | Interpretation unclear 4 possibilities: |
| Anti-HBc | Positive | 1. Resolved infection (most common) |
| Anti-HBs | Negative | 2. False positive |
| 3. “Low level” chronic infection | ||
| 4. Resolving acute infection |
From: Interpretation of hepatitis B serologic test results. Centers for Disease Control and Prevention website. www.cdc.gov. Accessed June 27, 2013.
In acute hepatitis B, medical attention is not sought early. In such cases the HBsAg may have already disappeared. The anti-HBs will not yet have emerged. Thus the sole viral marker may be anti-HBc. This same serologic pattern may be seen years after infection when the titer of anti-HBs is low. Sorting out the difference between late resolved hepatitis B and the period in acute hepatitis B described above can be achieved by testing for anti-HBc IgM which will be positive during this so-called “window period” of acute hepatitis B.
Chronic Hepatitis B
Chronic hepatitis B is characterized by persistence of HBsAg for a period longer than 6 months with positive anti-HBc (IgG), and negative anti-HBs. An additional antigen-antibody system plays a role in patients with chronic hepatitis B and requires mention: the hepatitis B e antigen (HBeAg) and its antibody (anti-HBe). HBeAg positivity in chronic hepatitis B usually indicates active viral replication and significant liver injury. In time, HBeAg may be lost, replaced by its antibody, anti-HBe. This transformation is often associated with lower level infection (less viral replication) or HBV DNA, lower AST and ALT values, and less (or no) hepatic inflammation.
Reactivation Hepatitis B
Hepatitis B reactivation is a sudden increase in hepatitis B virus (HBV) replication or the reappearance of active inflammatory disease of the liver in a patient with previously documented resolved HBV, or with the inactive HBsAg carrier state. Reactivation is usually triggered by immunosuppression in the host, which can occur following the use of chemotherapeutic agents for malignancy and following therapy for autoimmune diseases or organ transplantation.
Reactivation can also occur spontaneously. The extent of clinical manifestation from reactivation HBV can vary from a transient, clinically silent disease to severe or acute liver failure. A chronic infectious state can also be seen following HBV reactivation. Diagnosis of HBV reactivation depends on the HBV disease state before activation. In a patient with resolved infection (negative HBsAg and positive anti-HBs), reactivation is indicated by the decline in anti-HBs and the reappearance of HBsAg. In patients with quiescent HBV with positive HBsAg, reactivation is diagnosed by a rise in the serum HBV DNA (>1 log10 IU/mL) or a rise in the serum ALT levels (>3 times baseline). Reappearance of HBeAg in a patient with previous negative HBeAg also indicates HBV reactivation.
Role of HBV DNA Assays, HBV Genotypes and Liver Biopsy in Chronic Hepatitis B
HBV DNA level plays several important roles in chronic hepatitis B. It is the most important factor for predicting the progression to cirrhosis, helps to determine the need for treatment in HBeAg negative patients, and also plays a crucial role in estimating the response to treatment. Up to 8 HBV genotypes, labeled from A to H, have been identified. Recent studies have shown that some genotypes are associated with early HBeAg seroconversion, less progression to cirrhosis and hepatocellular carcinoma, and may also predict the response to treatment with interferon. These concepts and exceptions are discussed more fully in the Hepatitis B chapter. A clinical practice guideline on viral hepatitis B has provided additional information on laboratory testing in various contexts of hepatitis B infection.7
Resolved Hepatitis B and Immunization Status
As indicated in Table 6, an individual with resolved hepatitis B infection almost always has anti-HBc and anti-HBs. An individual successfully immunized against hepatitis B expresses only anti-HBs. Confusion may occasionally arise in the interpretation of hepatitis B tests in a patient who has recovered from hepatitis B many years ago and who has a low or absent level of measurable anti-HBc.
Hepatitis C
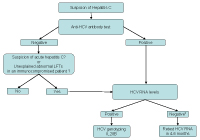
Because hepatitis C infection usually produces no symptoms, or only mild, nonspecific, flu-like symptoms, it is infrequently diagnosed in the acute phase. The virus clears spontaneously in about 15% of infected patients. Although generally helpful for the diagnosis of chronic infection, antibody tests are often not useful for diagnosis of acute hepatitis C virus (HCV) infection because the emergence of the antibody is delayed for several months after infection. To test for possible acute HCV infection, measurement of HCV RNA should be performed (Table 7). See the Disease Management chapter on Hepatitis C for further details.
Table 7: Hepatitis C Testing
| Test | Source | When To Order |
|---|---|---|
| Anti-HCV EIA | Patient immune system | Suspect HCV |
| HCV RNA PCR | HCV virus | Confirm current infection – If anti-HCV positive Or if acute HCV suspected Or in immunocompromised HCV suspect |
| HCV genotype | HCV virus | If HCV RNA positive and treatment contemplated |
| IL28B | Patient DNA | If genotype I HCV and treatment contemplated |
HCV, hepatitis C virus; EIA, enzyme immunoassay; PCR, polymerase chain reaction.
To test for chronic HCV infection, immunologic response to infection (antibodies) and viral assays are used. The most commonly used anti-HCV antibody test is an enzyme immunoassay with a specificity of greater than 99%. An individual with risk factors, elevated liver tests, and a positive anti-HCV has an overwhelming chance of HCV infection.
False-positive anti-HCV antibodies are occasionally encountered. Confirmation of chronic hepatitis C infection is obtained by the direct measurement of viral products in serum (HCV RNA). HCV RNA in serum definitively establishes the presence of HCV infection and is recommended in all patients with a positive anti-HCV test. Some clinicians have questioned whether the initial screening test for HCV should be an HCV RNA test or an antibody test. Currently, however, because of cost considerations, the initial test for HCV remains an anti-HCV antibody test.
False-negative anti-HCV tests can occur in two clinical contexts: in a patient with a recent infection, in an immunocompromised individual, or an individual receiving hemodialysis. HCV RNA testing is recommended in patients with negative anti-HCV antibody tests but who have liver disease of unknown etiology and are also immunocompromised.8 In addition, all potential organ donors should be tested for HCV RNA. Figure 1 gives a simplified diagnostic algorithm for hepatitis C.
Once the presence of HCV is established, the genotype should be determined. There are 6 major HCV genotypes (1-6). Genotyping continues to gain importance for treatment determinations. This is discussed more fully elsewhere in the Hepatitis C chapter.
Role of IL28B Genotype in Hepatitis C
Current guidelines do not routinely recommend interleukin 28B (IL28B) genotype testing.8 Nevertheless, it is commonly ordered to obtain information about the probability of treatment response and the duration of treatment. We recommend one-time testing of IL28B in every patient who is infected with genotype-1 hepatitis C who is also a candidate for treatment.
IL28 is a cytokine that plays an important role in the defense against viral infection. It belongs to the IL10 interferon family and, in response to a virus, helps to upregulate the inflammatory potential and the innate immunity. IL28 has two isoforms, namely IL28A and IL28B. The gene for IL28B resides on chromosome 19. Recent studies have identified a single nucleotide pleomorphism near the IL28B gene that can predict the response to treatment in hepatitis C. Three genotypes exist as a result of the nucleotide pleomorphism. They are the CC, CT, and TT genotypes. Among patients who spontaneously clear HCV virus, the CC genotype has been shown to be present more than twice as frequently than the other genotypes. In addition, patients with the CC genotype also show a much better response to treatment with anti-viral therapy as compared with the CT or TT genotype. Those with TT have the least response to treatment. This pattern has been observed among all ethnic groups.
Iron and Copper Overload Diseases
Diseases characterized by iron overload and copper overload are discussed in detail in the Disease Management (Inherited Metabolic Liver Diseases: Hemochromatosis, Wilson Disease). A practice guideline has been published.9
Iron Tests
Excess iron may accumulate in the liver and other organs for a variety of reasons. Some individuals have a genetic disorder while others may accumulate too much iron for other reasons. Among the genetic iron-overload conditions, the most common in individuals of Northern European ancestry is related to an autosomal recessive disorder, hereditary hemochromatosis. Before ordering tests it is important to be clear about what question is being asked. Most of the time the question is: Does my patient have iron overload?
This question should be entertained in the following situations:
- Any adult with liver disease, especially men and post-menopausal women
- Patients with symptoms suggestive of or having a family history of HH
The initial evaluation for iron overload includes measurement of serum ferritin, iron, iron-binding capacity, and transferrin saturation levels. Transferrin saturation less than 45%, in addition to normal serum ferritin level usually rules out iron overload (negative predictive value of 97%), and no further testing is necessary. Transferrin saturation greater than 45% and/or a serum ferritin above normal level warrants further investigation.9 However, these thresholds are low, and most patients who exceed these limits will not prove to have iron overload as explained below.
Limitations of Serum-Based Tests of Iron Overload
Because both iron and ferritin are stored in liver cells, any condition that results in hepatocyte injury and release of intracellular contents into the blood will falsely raise iron, transferrin saturation, and ferritin levels. Therefore, in acute hepatic injury these tests will falsely suggest iron overload. Acute inflammation outside the liver may also falsely elevate the results of serum-based iron tests. Tests of serum ferritin levels, iron, iron-binding capacity, and percentage saturation determined in the setting of markedly elevated aminotransferase levels (AST and ALT), such as those seen in acute viral hepatitis or massive hepatic necrosis, will be identical to those seen in hemochromatosis. Iron studies cannot be interpreted in the face of major elevations of transaminase levels.
Normal serum iron studies do not preclude future iron overload in the genetically susceptible individual. In a young patient with this condition who has not yet had enough time to accumulate iron (especially the premenopausal woman), screening tests for iron overload may be normal, even though the individual is at risk for the subsequent development of iron overload.
When iron overload is found or suspected, the question may become:
Does my patient have hereditary hemochromatosis?
This question should be entertained in:
- Any patient with elevated iron/total iron-binding capacity ferritin values
- Those with a family history of liver disease or of hemochromatosis
It has been known for years that many cases of hemochromatosis are inherited as an autosomal recessive trait. In many cases, a defective gene called the HFE gene is implicated. The presence of this inherited gene results in the production of a protein in which a tyrosine amino acid rather than a cysteine amino acid is present at position 282 of the HFE protein. A second missense gene that results in an aspartic acid (instead of histidine) at position 63 of the same protein may increase iron absorption in some patients. The abnormalities are called C282Y and H63D mutations respectively. Most individuals of Northern European descent with hereditary hemochromatosis usually have two abnormal genes (homozygosity). Most often, two C282Y genes are present, but occasionally a compound heterozygote (C282Y-H63D) will also have excess iron. Homozygosity for H63D does not usually result in excess iron absorption (Table 8).
Table 8: Guidance for the Likelihood of Iron Accumulation with Various HFE Patterns
| HFE Finding | Likelihood of Iron Overload |
|---|---|
| Wild type/wild type (no abnormal genes) | Nil |
| Wild type/C282Y | Nil |
| C282Y/C282Y (C282Y homozygote) | High |
| Wild type/H63D | Nil |
| H63D/H63D (H63D homozygote) | Low |
| C282Y/H63D (compound heterozygote) | Moderate |
Confirming a Diagnosis of Hemochromatosis and the Role of Liver Biopsy
Homozygosity for C282Y and compound heterozygosity for C282Y/H63D are diagnostic of HH and a liver biopsy with hepatic iron index (HII) estimation, which was previously the criteria for diagnosis, is no longer needed to confirm the diagnosis of HH in these patients. In addition, HFE gene mutation testing is indicated in all first-degree relatives of patients with hemochromatosis.9 However, it must be remembered that many individuals have iron overload with normal HFE protein. Pre-menopausal women with C282Y homozygosity most often have no iron accumulation. Finally, there is incomplete penetrance of iron overload in many C282Y homozygotes. In other words, expression of disease may not occur despite having the genetic susceptibility.
HFE gene mutation analysis does not establish either the presence or the degree of liver fibrosis or cirrhosis. Studies have shown that patients with serum ferritin less than 1,000 ng/mL are less likely to have cirrhosis in HH.10 A liver biopsy is thus indicated in patients with elevated ferritin greater than 1,000 ng/mL or having abnormal liver enzymes. This serves two purposes, determining fibrosis and providing an assessment of iron stores. Because there is an age-dependent increase in hepatic iron in normal individuals, it is necessary to create an index that takes this into account. HII is calculated as follows:
HII = hepatic iron concentration(mcmol/g dryweight) ÷ patient age(years)
HII less than 1.9 is normal; values greater than 1.9 are seen in hemochromatosis.9 A caveat to this would be in cirrhotic livers, which have the tendency to rapidly accumulate iron in liver disease of other etiologies and cause elevation of HII to a level greater than 1.9. Newer techniques, such as the HIC estimation by proton transverse relaxation time determined by MRI, could be an alternative to liver biopsy, and studies have shown good correlation between the tests. It must be remembered that bone marrow iron stores are not adequate to assess total body iron stores. Cases of hemochromatosis with absent stainable bone marrow iron have been reported.
Copper Tests
Although copper may accumulate to moderate excess in the liver in any chronic cholestatic liver condition, it does not appear to be injurious in these conditions. Wilson disease is the main disease in which pathologic copper deposition results in serious liver injury, cirrhosis, and death. In Wilson disease, copper also accumulates in the basal ganglia of the brain, where it produces a wide gamut of neurologic abnormalities. Patients may present with liver disease, brain disease, or both. This disorder is discussed in more detail in the Disease Management (Inherited Metabolic Liver Diseases: Wilson’s Disease).
Wilson disease is rare. Untreated, it is usually fatal before the patient is aged 40 years. Therefore, it is most appropriate to consider this potential cause in a child or young adult with otherwise unexplained liver disease. However, a diagnosis of Wilson disease should not be excluded based on age alone. Laboratory diagnosis is most often based on the finding of a low ceruloplasmin level. Serum ceruloplasmin level of less than 5 mg/dL strongly suggests Wilson disease while any subnormal level warrants further evaluation. Most acute and chronic liver diseases cause the ceruloplasmin level to elevate. There are a few exceptions to this. A patient with acute fulminant liver failure of any sort may no longer have a liver capable of ceruloplasmin synthesis, so that patient may have a low serum level. Similarly, the patient with terminal end-stage liver disease may have a falling ceruloplasmin level. Finally, a few individuals have congenital hypoceruloplasminemia without copper accumulation and are healthy. At the same time, it must also be remembered that a normal serum ceruloplasmin level does not exclude Wilson disease.
In patients in whom Wilson disease is suspected, in addition to serum ceruloplasmin, 24-hour urinary copper levels and slit lamp examination to look for Kayser-Fleischer (KF) rings should be obtained. A serum ceruloplasmin level less than 20 mg/dL, 24-hour urine copper greater than 40 mcg, and the presence of KF rings confirms the diagnosis of Wilson disease. No further testing such as a liver biopsy is needed in this setting.11
Copper is present in the serum in two forms: copper that is bound to ceruloplasmin, and free copper or the non-ceruloplasmin bound copper. The total serum copperlevel is the sum of the levels of these two forms of copper and is usually low in those with Wilson disease. This is partly explained by the decrease in the ceruloplasmin bound copper level that results from a reduction in the ceruloplasmin level in Wilson disease. However, the serum free copper level is typically elevated to ≤25 mcg/dL in patients with Wilson disease and may be approximated as follows:
Serum free copper level = Total serum copper level (ug/dl)l − (3 x serum ceruloplasmin level (mg/dL))
A practical algorithm on the diagnostic tests for Wilson disease in shown in Table 9.11
Table 9: Diagnostic Tests for Wilson Disease11
| Level 1 Tests | Level 2 Tests | Level 3 Tests |
|---|---|---|
| Low serum ceruloplasmin level (<20 mg/dL) | Liver histopathology and stainable copper | Ultrastructural study of hepatocytes |
| Kayser-Fleischer rings | Liver copper concentration (>250 µg/g dry weight) | Mutational gene analysis for Wilson disease |
| Raised serum-free copper level (non-ceruloplasmin-bound) (>25 µg/dL) | Incorporation of radiocopper into ceruloplasmin | |
| 24-hr urinary copper (>100 µg/24 hr) |
Autoimmune Liver Diseases
The two most common forms of autoimmune liver disease are autoimmune chronic hepatitis and PBC. Ninety percent of those with each disorder are women. Autoimmune hepatitis (AIH) is characterized by very high serum aminotransferase (ALT and AST) levels, whereas PBC is a cholestatic disorder with predominant elevations of the alkaline phosphatase level. Each is associated with autoantibodies in the serum. The treatment for each is different, so accurate diagnosis is essential. Table 10 contrasts the laboratory findings of these two autoimmune liver disorders.
Table 10: Contrasting Features of Two Autoimmune Liver Diseases
| Feature | Autoimmune Chronic Hepatitis | Primary Biliary Cirrhosis |
|---|---|---|
| AST, ALT | 7-10 times upper limit of normal (ULN) | 1-3 times ULN |
| Alkaline phosphatase | 1-3 times ULN | 2-10 times ULN |
| Anti-smooth muscle antibody positive | 90% (usually high titer) | 10%-20% (usually low titer) |
| Anti-mitochondrial antibody positive | 10%-20% (usually low titer) | 90%-100% (usually high titer) |
| Liver-kidney microsomal antibody positive | Positive in some cases in which smooth muscle antibody is negative (rare in North America) | Negative |
ALT, alanine aminotransaminase; AST, aspartate transaminase.
Interpretation of autoimmune markers in a patient with liver disease is highly context-dependent. Autoantibodies are common in low titer in a number of acute and chronic liver conditions, such as viral hepatitis. Therefore, the finding of autoantibodies in low titer is not sufficient evidence with which to make a diagnosis of autoimmune chronic hepatitis or PBC. At the same time, low titers do not exclude the diagnosis.
Autoimmune Hepatitis
AIH should be rapidly recognized by its propensity to occur in women (90%) and to be associated with high transaminase levels (200 IU/mL or higher). In this disease, elevations of the gamma globulins (especially IgG) are pronounced. A myriad of autoimmune markers may be positive in autoimmune chronic hepatitis, but only a few serological markers have to be assessed: anti-smooth muscle antibody, antinuclear antibody, liver-kidney microsomal antibody and anti-liver cytosol type 1 antibody. High titers of antibodies are suggestive of but on their own they do not establish a diagnosis of AIH.
The diagnosis of AIH can be difficult at times and various factors need to be taken into account. Clinical criteria are usually sufficient to make a diagnosis of or to exclude AIH. Scoring systems have been developed to assist in establishing a diagnosis of AIH.12,13 Exclusion of other liver diseases should be undertaken as part of the work up. A liver biopsy at presentation is recommended to establish the diagnosis of AIH and to make treatment decisions.14
Primary Biliary Cirrhosis
PBC is an autoimmune liver disease that characteristically involves the intrahepatic small bile ducts. In this condition, serum-based liver tests reveal a predominant elevation of the alkaline phosphatase level. It is associated with the elevation of an autoantibody in high titer known as the anti-mitochondrial antibody (AMA). It has a high sensitivity and a very high specificity. It is reported to be seen in less than 1% of normal people. However AMA has been shown to be present in increased frequency in relatives of patients with PBC. One study showed that the frequency of positive AMA among first-degree relatives of patients with PBC was 13% as compared with 1% in controls.15 Though positive AMA antibodies may suggest susceptibility to development of PBC, they, on their own even in high titers, do not establish a diagnosis of PBC. Ultrasound or other imaging techniques are necessary in all patients to exclude bile duct obstruction as the cause of cholestasis. Presence of predominant alkaline phosphatase elevation and positive AMA antibody establishes the diagnosis of PBC.16 Liver biopsy is indicated if the AMA is negative or is in low titers and if associated AIH or NAFLD is suspected. Occasionally, a patient may have features of both autoimmune chronic hepatitis and PBC known as AIH/PBC overlap syndrome. PBC is discussed more in detail elsewhere in the Disease Management (“Primary Biliary Cirrhosis, Primary Sclerosing Cholangitis, and Other Cholestatic Liver Diseases“).
Non-Alcoholic Fatty Liver Disease
NAFLD is the most common cause of mildly elevated liver enzymes. Please see the chapter on Non-Alcoholic Fatty Liver Disease in Disease Management. NAFLD is defined as the accumulation of fat in the liver in the absence of conditions that cause secondary fat accumulation such as alcoholic hepatitis, medications, metabolic disorders or viral hepatitis.17 Two types of NAFLD have been described, non-alcoholic fatty liver and non-alcoholic steatohepatitis. The latter has evidence of hepatocellular injury in addition to fat accumulation. Patients with NAFLD are non-alcoholic, usually obese, and have a high BMI.
Liver tests are unreliable guides to the presence or absence of fatty liver disease. When elevated, enzymes show hepatocellular pattern, often with an AST/ALT ratio of less than 1. However, they can be normal. Therefore, liver tests are not useful to make a diagnosis of NAFLD. A history of significant alcohol intake can reliably distinguish between alcoholic fatty liver disease and NAFLD. Imaging is performed to demonstrate the presence of fat in the liver. Liver biopsy is indicated if competing etiologies cannot be ruled out, if a co-existing liver disease is suspected, and for patients at risk of developing cirrhosis.17
A scoring system has been developed to identify patients with liver fibrosis in NAFLD.18 This scoring system comprises of six variables namely: age, hyperglycemia, body mass index, platelet count, albumin, and AST/ALT ratio. The system has been shown to distinguish patients with NAFLD and with or without advanced fibrosis accurately. Certain biomarkers such as serum CK18 have been shown to predict the presence of hepatocellular injury in NAFLD, but further studies are needed to establish their utility.
Noninvasive Tests for Liver Fibrosis and Cirrhosis
Liver biopsy is the gold standard for determining the stage of liver fibrosis and cirrhosis. However, it is invasive and can cause significant complications and sampling error, the latter due to the non-uniform distribution of fibrosis in the liver. In recent years, a number of noninvasive tests have been developed and are being studied to assess liver fibrosis and cirrhosis. Among these, the most widely studied and promising noninvasive tests are hepatic elastography and the serologic markers of fibrosis. Serologic markers can be further divided into direct markers and indirect markers. Direct serologic markers are those that are associated with the deposition of matrix and include procollagen type III amino-terminal peptide (P3NP), type I and IV collagens and matrix metalloproteinases among others.19 P3NP is found to be the most promising among these markers. It is elevated in both acute and chronic liver disease. Studies have also shown that the serum levels of P3NP reflect the degree of fibrosis in chronic liver disease. However, the test is currently not readily available in commercial laboratories and has not yet been validated for use.
Hepatic elastography is a noninvasive imaging technique used to determine the degree of fibrosis of the liver. Most frequently, ultrasound-based elastrography is performed. It uses a device called Fibroscan which transmits low-frequency waves into the liver. The waves’ velocities are then recorded and are shown to correlate with the liver stiffness. It can be performed either by an ultrasound or MRI. Studies have shown that ultrasound elastography has excellent diagnostic accuracy to diagnosing cirrhosis but does not perform as well to assess fibrosis. Magnetic resonance elastography has been shown to be the most promising noninvasive test as studies have shown that it can assess both the degree of fibrosis in addition to diagnosing cirrhosis.20 However, its use may be limited by its high cost. In addition, these tests are not yet FDA-approved to be used in the United States. Therefore, liver biopsy still remains the most important tool in the assessment of liver fibrosis and cirrhosis, though the need for it may be significantly decreased in the future with the further development and validation of noninvasive tests.
Conclusion
Laboratory assessment of the patient with suspected or clinically obvious liver disease is context dependent and has to be individualized. It is useful to categorize liver diseases into three broad categories: hepatocellular, cholestatic, and infiltrative. Once the liver disease has been categorized, following appropriate diagnostic algorithms driven by a good history and physical examination are the easiest and the most reliable ways to obtain the correct diagnosis.
References
- American Gastroenterological Association. Medical position statement: evaluation of liver chemistry tests. Gastroenterology 2002; 123:1364–1366.
- Green RM, Flamm S. AGA technical review on the evaluation of liver chemistry tests. Gastroenterology 2002; 123:1367–1384.
- Carey WD. How should a patient with an isolated GGT elevation be evaluated? Cleve Clin J Med 2000; 67:315–316.
- Kim HC, Nam CM, Jee SH, Han KH, Oh DK, Suh I. Normal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort study [published online ahead of print March 17, 2004]. BMJ 2004; 328:983. doi:10.1136/bmj.38050.593634.63.
- Ruhl CE, Everhart JE. Upper limits of normal for alanine aminotransferase activity in the United States population. Hepatology 2012; 55:447–454.
- O’Shea R, Dasarathy S, McCullough AJ; Practice Guideline Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Alcoholic liver disease. Hepatology 2010; 51:307–328.
- Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology 2009; 50:661–662.
- Ghany MG, Nelson DR, Strader DB, Thomas DL, Seeff LB; American Association for Study of Liver Diseases. An update on treatment of genotype 1 chronic hepatitis C virus infection: 2011 practice guideline by the American Association for the Study of Liver Diseases [published online ahead of print September 26, 2011]. Hepatology 2011; 54:1433–1444. doi:10.1002/hep.24641.
- Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS; American Association for the Study of Liver Diseases. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology 2011; 54:328–343.
- Morrison ED, Brandhagen DJ, Phatak PD, et al. Serum ferritin level predicts advanced hepatic fibrosis among U.S. patients with phenotypic hemochromatosis. Ann Intern Med 2003; 138:627–633.
- Roberts EA, Schilsky ML; American Association for Study of Liver Diseases (AASLD). Diagnosis and treatment of Wilson disease: an update. Hepatology 2008; 47:2089–2111.
- Alvarez F, Berg PA, Bianchi FB, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol 1999; 31:929–938.
- Hennes EM, Zeniya M, Czaja AJ, et al; International Autoimmune Hepatitis Group. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology 2008; 48:169–176.
- Manns MP, Czaja AJ, Gorham JD, et al; American Association for the Study of Liver Diseases. Diagnosis and management of autoimmune hepatitis. Hepatology2010; 51:2193–2213.
- Lazaridis KN, Juran BD, Boe GM, et al. Increased prevalence of antimitochondrial antibodies in first-degree relatives of patients with primary biliary cirrhosis. Hepatology 2007; 46:785–792.
- Lindor K, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ; American Association for Study of Liver Diseases. Primary biliary cirrhosis. Hepatology2009; 50:291–308.
- Chalasani N, Younossi Z, Lavine JE, et al; American Association for the Study of Liver Diseases; American College of Gastroenterology; American Gastroenterological Association. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association [published correction appears in Am J Gastroenterol 2012; 107:1598]. Am J Gastroenterol 2012; 107:811–826.
- Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007; 45:846–854.
- Carey E, Carey WD. Noninvasive tests for liver disease, fibrosis, and cirrhosis: is liver biopsy obsolete? Cleve Clin J Med 2010; 77:519–527.
- Godfrey EM, Patterson AJ, Priest AN, et al. A comparison of MR elastography and 31P MR spectroscopy with histological staging of liver fibrosis [published online ahead of print July 1, 2012]. Eur Radiol 2012; 22:2790–2797. doi:10.1007/s003330-012-2527-x.